Application of Intraoperative Three-Dimensional Computed Tomography Reconstruction to Evaluate the Effects of Different Ventilation Strategies on Lateral Atelectasis during One-Lung Ventilation
Application of Intraoperative Three-Dimensional Computed Tomography Reconstruction to Evaluate the Effects of Different Ventilation Strategies on Lateral Atelectasis during One-Lung Ventilation
Gianluca Ancona1, Angelica Ancona2, Shangqing Xu3,4, Biao Han3,4,5, ning wei3,6,7,lixin liu3, ruijiang lin3, Wenteng Hu3, Peng Yue3, Xiong Cao3, Hongbing Wang3 ,Yang Liangliang4,Xiang Ma3,Zhiwei Han3,Yatao Liu3, Yongqi Wang3, Diego Gonzalez-Rivas3,6, Minjie Ma3,5,6,7*
1. Complex Operating Unit of Thoracic Surgery, Morelli Hospital, ASST Valtellina e alto Lario, Sondalo, Italy,
2 Department of Anesthesia analgesia Intensive Care and Emergency, University Hospital Policlinico ‘Paolo Giaccone’, 90127 Palermo, Italy,
3 Department of Thoracic Surgery, ‘The First Hospital of Lanzhou University’ Lanzhou, China?
4 Skills Training Center, The First Clinical Medical College of Lanzhou University Lanzhou , China,
5 The First Clinical Medical College of Lanzhou University Lanzhou, China,
6 The International Science and Technology Cooperation Base for Development and Application of Key Technologies in Thoracic Surgery Lanzhou, China; 7 Control Center of Thoracic Surgery of Gansu Province Lanzhou, China;
Correspondence to: Minjie Ma Department of Thoracic Surgery, The First Hospital of Lanzhou University, Lanzhou 730000, china.
Copyright
© 2025 Minjie Ma. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 27 Jan 2025
Published: 05 Feb 2025
ABSTRACT
Objective: To investigate the effect of intraoperative anesthetic ventilation with high positive end-expiratory pressure, low tidal volume, and high respiratory rate on the prevention of lateral atelectasis during one-lung ventilation in pulmonary surgery.
Methods: One hundred patients who underwent computed tomography for the intraoperative localization of pulmonary nodules between October 2021 and March 2022 were included. We assigned 50 patients each to the experimental group and control group on the basis of intraoperative anesthetic ventilation. High positive end-expiratory pressure, low tidal volume and high respiratory rate was used in the experimental group, whereas the conventional protective ventilation strategy was used for the control group.
Results: Both the groups completed surgery successfully; the degree of pulmonary atelectasis in the ventilated side of the lung in the experimental group was significantly lower than that in the control group (P < 0.05).
Conclusion: The use of high positive end-expiratory pressure + low tidal volume + high respiratory rate can reduce the degree of pulmonary atelectasis during one-lung ventilation in thoracic surgery and can thus effectively improve the safety of surgery.
Application of Intraoperative Three-Dimensional Computed Tomography Reconstruction to Evaluate the Effects of Different Ventilation Strategies on Lateral Atelectasis during One-Lung Ventilation
An increasing number of studies have reported that postoperative lung injury (PLI) during thoracic surgery is a major cause of postoperative pulmonary complications Lung injury is mainly caused by surgical trauma, alveolar reopening, and concomitant ischemia–reperfusion injury.1 Intraoperative atelectasis is a central cause of these injuries, especially in the ventilated lungs; however, the actual working status and imaging findings of the ventilated side of the lung during surgery have not yet been reported. However, we detected atelectasis on the ventilated side when we used chest computed tomography (CT) to locate pulmonary nodules in the operating room. We then used patients’ intraoperative CT data to perform three-dimensional (3D) reconstruction by using Mimics Medical 21.0 (Materialise Corp.Belgium) to observe atelectasis and compare the site and degree of atelectasis with those observed on the preoperative CT image. In this study, we explored the causes of atelectasis occurring on the ventilated side of a single lung during thoracic surgery by changing ventilation settings during intraoperative anesthesia and employing different ventilation strategies to reduce the degree of atelectasis that occurs intraoperatively.
1 Data and methods
1.1 Study participants
We included 100 patients who underwent intraoperative CT for the localization of pulmonary nodules during compound procedures from October 2021 to March 2022 in this study and randomly divided them into experimental and control groups.
1.1.1 Patient inclusion criteria
(1) Being aged 20 to 75 years;
(2) Having undergone single-port thoracoscopic lung surgery;
(3) Having undergone intraoperative CT for the localization of pulmonary nodules.
1.1.2 Patient exclusion criteria
(1) Having a disease of key organs including the heart, lungs, or kidneys and thus being unable to tolerate surgery;
(2) Lacking surgical indications such as pneumonia or other tumors and distant metastases;
(3) Having undergone two-port or three-port thoracoscopy or open-chest or intraoperative conversion to open-heart surgery.
1.2 Anesthesia
An intravenous infusion of 50 mg of flurbiprofen ester and an intravenous injection of 0.5 mg of pentobarbital hydrochloride were administered 30 minutes before the surgery. Upon entering the operating room, routine monitoring of electrocardiography (ECG), blood pressure, and pulse oximetry (SpO2) was performed using a Philips IntelliVue MP50 cardiac monitor. Anesthesia induction was conducted by administering intravenous dexamethasone 10 mg, propofol 2 mg/kg, sufentanil 0.5 μg/kg, and rocuronium bromide 0.6 mg/kg. After the insertion of a double-lumen tracheal tube, breathing was controlled using a Dräger Fabius GS anesthesia machine. Monitoring of arterial pressure was performed via radial artery puncture, and placement of a central venous catheter was achieved through internal jugular vein puncture. Anesthesia maintenance involved continuous infusion of propofol at a rate of 4-12 mg/kg/h and remifentanil at a rate of 0.25-4 μg/kg/min using an electronic syringe pump manufactured by Smiths. Inhalation of sevoflurane was employed as an adjunct when necessary. All patients underwent intubation using either an F37 or F35 double-lumen tracheal tube, with confirmation of placement performed using fiberoptic bronchoscopy. In all cases, the pleural cavity was opened on the operative side, and one-lung ventilation (OLV) of the healthy lung was initiated before entering the chest.
In the experimental group, high positive end-expiratory pressure (PEEP) + low tidal volume + high respiratory rate was applied along with the following ventilator settings: frequency = 13–20 times/min, tidal volume = 6–8 mL/kg, and PEEP = 10–20 cmH2O.
The conventional ventilation strategy was applied in the control group, and control ventilator settings were as follows: frequency = 12 times/min, tidal volume = 10–12 mL/kg, and PEEP = 5–10 cmH2O.2-7
All the patients underwent a CT scan of the chest within 10 min of the opening of the pleural cavity on the operative side. Before the scan, to prevent the weight of the lobe on the operative side from affecting the ventilated side during the localization of the site of the lung lesion, the surgical incision was closed on the operative side and negative pressure suction was used to reopen the lung. The pleura of the lung wall with the visceral pleura was apposed and the lung on the ventilated side was controlled to be in an air intake state by using the anesthesia system during the scan.
1.3 Observation indices
1.3.1 General data
We collected information on patients’ age, sex, lesion location, and pathological lesion type.
1.3.2 CT data
CT data were employed for lung reconstruction by using Mimics Medical 21.0 (Materialise Corp.Belgium) and lobe segmentation, and extracted lung volume values were used to determine statistical changes in preoperative and postoperative OLV volumes.
1.4 Statistical methods
We first calculated the preoperative and intraoperative lung volumes of each lung lobe in the control group by using CT 3D reconstruction calculations and concluded that the intraoperative patients had intraoperative pulmonary atelectasis on the ventilated side. We subsequently improved intraoperative ventilation to determine if this can reduce pulmonary asplenia on the ventilated side of a lung. The data were statistically analyzed using SPSS26.0 software. Measurement data are expressed as the mean ± standard deviation (x ± s), and a t test was used for between-group comparison; count data are expressed as the frequency or percentage, and rates were compared using a chi-square test or Fisher’s exact probability test. P < 0.05 indicated a statistically significant difference.
2 Study results
2.1 Comparison of the general information of the two groups
A total of 50 patients each were included in the experimental and control groups. No significant differences (P > 0.05) in age, sex, lesion location, surgical procedure, and pathological lesion type were noted between the groups (Table 2).
2.2 Preoperative and intraoperative lung volume changes in the control group
2.2.1 Left-sided lung volume
In the 29 patients who underwent left-sided OLV, the total volume of the left lung changed from 2546.97 ± 353.73 cm3 preoperatively to 2055.13 ± 301.42 cm3 intraoperatively. The intraoperative total volume was significantly lower than the preoperative total volume (P < 0.001), indicating the presence of atelectasis on the ventilated side of the left lung. The volume of the left upper lung lobe was 1512.25 ± 209.87 cm3 preoperatively and 1533.32 ± 222.93 cm3 intraoperatively, indicating no significant change between the values (P = 0.712). In some patients, the intraoperative volume was higher than the preoperative volume, probably due to intraoperative transitional ventilation expansion. The preoperative volume of the left lower lobe of the lung (1036.75 ± 146.92 cm3) was significantly higher than its total intraoperative volume (521.81 ± 90.04 cm3; P < 0.001). This indicated the presence of atelectasis in the left lower lobe of the ventilated side of the lung (Table 2 and Figure 1,2,3).
Table 1. Comparison of general information of patients in the experimental group and control group
Table 2. Comparison of the degree of interlobular atelectasis in patients in the control group
Fig. 1 Preoperative images of the left lung in the control group.
Fig. 2,3 Intraoperative images of the left lung in the control group
2.2.2 Right-sided lung volume
In the 21 patients who received intraoperative right-sided lung ventilation, the preoperative total volume of the right lung (2678.26 ± 343.27 cm3) was significantly higher than its intraoperative total volume (1990.31 ± 218.20 cm3; P < 0.001, indicating the presence of atelectasis on the ventilated side of the lung. The preoperative and intraoperative volumes of the right upper lung lobe were 1069.76 ± 141.30 cm3 and 1087.13 ± 146.63 cm3, respectively; these values did not significant differ from each other (P = 0.696). The preoperative and intraoperative volumes of the right middle lung lobe were 428.88 ± 110.88 and 258.80 ± 47.17 cm3, respectively; the intraoperative volume was significantly lower than the preoperative volume (P < 0.001), indicating the presence of atelectasis in the right middle lobe of the ventilated side of the lung. The preoperative volume of the right lower lobe was 1179.56 ± 135.70 cm3; the total intraoperative volume was 534.38 ± 66.97 cm3, which was significantly lower than the preoperative volume (P = 0.003), indicating the presence of atelectasis in the right lower lobe on the ventilated side of the lung(Figure 4,5,6).
Fig. 4 Preoperative images of the right lung in the control group.
Fig. 5,6 Intraoperative images of the right lung in the control group.
2.3 Comparison of the degree of interlobular atelectasis in the control group
2.3.1 Preoperative and intraoperative volumes of the left lung
In the 29 patients who underwent intraoperative left-sided lung ventilation, the ratios of the intraoperative volume to the preoperative volume of the upper and lower lobes of the left lung were 1.01 ± 0.24 and 0.51 ± 0.11, respectively. The results indicated that the change in the ratio of the preoperative volume to the intraoperative volume of the upper lobe was smaller than the change in the lower lobe, indicating that the degree of atelectasis in the lower lobe during left-sided OLV was greater than that in the upper lobe(Figure 7,8,9).
Fig. 7 Preoperative images of the left lung in the test group.
Fig. 8,9 Intraoperative images of the left lung in the test group.
2.3.2 Intraoperative and preoperative volumes of the right lung
In the 21 patients who underwent intraoperative right-sided lung ventilation, the ratio of the intraoperative volume to the preoperative volume of the right upper lobe was 1.02 ± 0.25. The ratios of the intraoperative volume to the preoperative volume of the right middle and lower lobes were 0.64 ± 0.18 and 0.55 ± 0.30, respectively. The results revealed that the preoperative volume of the right upper lobe was smaller than that of the middle lobe, and the preoperative volume of the lower lobe was smaller than that of the middle lobe. These results indicated that the degree of pulmonary atelectasis in the lower lobe was greater than that in the middle lobe after OLV, and the degree of pulmonary atelectasis in the middle lobe was greater than that in the upper lobe(Figure 10,11,12).
Fig. 10 Preoperative images of the right lung in the test group.
Fig. 11,12 Intraoperative images of the right lung in the test group
Please click here to view all figures and tables
2.4 Comparison of the degree of atelectasis between different lobes of the lungs in the experimental and control groups
2.4.1 Intraoperative and preoperative volumes of the upper and lower lobes between the groups
The ratio of the intraoperative volume to the preoperative volume of the upper lobe in the control group was 1.01 ± 0.02, which was not significantly different from that of 1.03 ± 0.03 in the experimental group (P = 0.78); the ratio of the intraoperative volume to the preoperative volume of the lower lobe in the control group was 0.51 ± 0.11, which was significantly different from that of 0.75 ± 0.15 in the experimental group. The ratio of the intraoperative volume to the preoperative volume of the lower lobe was significantly lower in the control group than in the experimental group (P < 0.001; Table 3).
2.4.2 Intraoperative and preoperative volumes of the upper, middle, and lower lobes between the groups
In the patients who underwent intraoperative right-sided lung ventilation, the ratios of the intraoperative volume to the preoperative volume of the upper lobe were 1.02 ± 0.03 and 1.03 ± 0.02, in the control group and experimental group, respectively; no significant difference between these values was noted (P = 0.20). The ratios of the intraoperative volume to the preoperative volume of the middle lobe were 0.64 ± 0.18 and 0.79 ± 0.21, in the control and experimental groups, respectively; these values significantly differed from each other (P = 0.017). The ratios of the intraoperative volume to the preoperative volume of the lower lobe were 0.55 ± 0.03 and 0.62 ± 0.07, in the control and experimental groups, respectively; these values significantly differed from each other (P < 0.001; Table 3).
Table 3. Comparison of the degree of atelectasis among different lobes of the lung in the experimental group and control group
Discussion
The incidence of PLI in thoracic surgery is 4.3%. PLI can lead to postoperative pulmonary complications, such as pneumonia and ARDS, prolong patients’ hospital stay, and lead to increased postoperative mortality.[1] PLI in thoracic surgery is considered to be induced by two-lung ventilation (TLV) before one-lung ventilation (OLV), followed by surgical trauma, alveolar reopening, and concomitant ischemia –reperfusion injury.[1] The main complication of ventilation pulses is intraoperative lung atelectasis, especially on the ventilated side, but the actual working status and imaging findings of the intraoperative lung on the ventilated side have not yet been reported. Therefore, we included 100 patients who underwent intraoperative CT scanning for the intraoperative localization of pulmonary nodules between 2021 and 2022 in the Department of Thoracic Surgery of the First Hospital of Lanzhou University in this study. We used original intraoperative CT data to perform 3D reconstruction by using Mimics software to observe pulmonary atelectasis, compared the site and degree of atelectasis by using preoperative CT data, and identified the intraoperative indicators of anesthesia to explore the causes of pulmonary atelectasis in the patients in the lateral recumbent position undergoing OLV during thoracic surgery.
Using preoperative and intraoperative CT scans, we discovered that the ventilated side of the lung is often in partial atelectasis during OLV. Moreover, the degree of atelectasis differed among different lobes on the ventilated side, and the intraoperative lung volume was smaller than the preoperative volume in both the groups. In both groups, the degree of atelectasis in the upper lobes of both the lungs was smaller than that in the middle and lower lobes, which may be related to the length and diameter of the ventilation tract and the bronchi of each lobe and the obstruction of secretion drainage. Airway resistance during ventilation was related to the length and diameter of bronchi, and the pressure in the airways of the middle and lower lobes was relatively higher than that in the upper lobes during ventilation; thus, the degree of atelectasis in the middle and lower lobes was more severe, whereas the upper lobes were less atelectatic or even transitionally inflated.
Among the many causes of pulmonary atelectasis during OLV, gravity is a crucial determinant of atelectasis on the ventilated side during OLV.8-10
The lung on the ventilated side is located in the lower part and the mediastinum is shifted by gravity, resulting in the smaller volume of the compressed lung on the healthy side. When the pleural cavity on the affected side is opened on the healthy side while the patient is in the lateral position, the negative pressure is reduced and the mediastinum loses its traction, further shifting to the healthy side. This leads to a reduction in the volume of the compressed lung on the ventilated side, resulting in restrictive atelectasis. Because of the effect of gravity, secretions and exudates in the airway and lung drain to the lowest point, resulting in obstructive atelectasis. In some procedures employing artificial pneumothorax, the effect is greater than that of the opening of the pleural cavity, resulting in pressure reduction on the ventilated side of the lung.
Intraoperative atelectasis can lead to a series of physiopathological changes, leading to lung injury and severe complications. During OLV, the ventilated lung becomes atrophied as a result of the elastic retraction force of the lung itself, the compression of the mediastinal septum, and the absorption of oxygen in the area with a low ventilation/blood flow ratio. When the lung reopens in the atrophied state, the corresponding alveoli are placed under considerable mechanical stress and tension, and strong shear forces are exerted on the adjacent alveoli, consequently damaging the adjacent nonatrophied alveoli. During OLV, if appropriate ventilation parameters are not set, repeated alveolar atrophy and reattachment during ventilation can result in alveolar injury.6, 11, 12 Hyperperfusion lung injury after lung atrophy3 and ischemia–reperfusion injury after lung reattachment exacerbate preexisting lung injuries.13-18
Prevention of atelectasis on the ventilated side during OLV is essential for preventing postoperative pulmonary complications.
Studies13, 18, 19 have concluded that PLI during OLV is directly induced through the overstretching of the lung tissue during mechanical ventilation therapy and is indirectly caused by inflammatory infections induced by multiple factors, which is called biological injury. Increasing the tidal volume and PEEP after OLV is widely considered to be the cause of lung hyperinflation on the ventilated side, which results in PLI and an intraoperative PEEP of <10 cmH2O.
Many studies have indicated that the use of high tidal volume ventilation during OLV can lead to lung injury. Furthermore, intraoperative mechanical ventilation using a small protected tidal volume (6–8 mL/kg) can significantly reduce the incidence of postoperative pulmonary complications in patients compared with the use of conventional unprotected high tidal volume (10–12 mL/kg) and can significantly improve the long-term prognosis of patients.2-4 Clinical studies have also demonstrated that high tidal volume mechanical ventilation during OLV was associated with high interleukin concentrations and a low oxygenation index in the postoperative bronchoalveolar lavage fluid as well as a high incidence of PLI in patients. These observations suggest a relationship between high tidal volume and PLI.20, 21
The currently used OLV ventilation protocol is based on a low tidal volume protective ventilation strategy for patients with an ideal body weight (tidal volume = 6 mL/kg) and includes the routine use of PEEP ventilation with a low inhaled oxygen concentration, low peak pressure, and low airway plateau pressure, which can prevent excessive and repetitive lung expansion, thus limiting high plateau pressure, providing adequate oxygenation, and significantly reducing patient PLI. The incidence of PLI is significantly lower in patients treated with the OLV protocol than that in patients treated using conventional ventilation.1, 5, 22
Other studies have revealed that low-tidal-volume lung protection protocols exacerbate pulmonary atelectasis during OLV,23 which is consistent with the findings of our intraoperative CT scan observations Although low-tidal-volume ventilation is effective as a component of OLV protective ventilation strategies,24, 25 it does not prevent postoperative pulmonary complications in the absence of appropriate PEEP.
When applied in standard ventilation, PEEP (5–10 cmH2O) cannot overcome the surface tension problem of atelectasis and can lead to excessive alveolar pressure in some inflated lobes, resulting in alveolar damage, ventilation-induced blood flow changes, and arterial oxygen saturation on the low side.7 Our study suggested that the distal lobe of the lung in the control group had a large degree of atelectasis, whereas the upper lobe had mild atelectasis and even excessive expansion. PEEP ventilation during OLV has a direct effect on alveolar gas exchange and pulmonary resuscitation compliance and has an indirect effect on systemic hemodynamic changes. When bilateral lung operation is transferred to OLV, pulmonary artery oxygenation is reduced and alveolar ventilation increases. With OLV, the oxygenation index does not significantly change during personalized PEEP ventilation. In standard PEEP ventilation, the oxygenation index exhibited a downward trend, and lung compliance was reduced to a certain extent. Following the application of optimal PEEP ventilation setting, the lung compliance increased significantly. Moreover, the personalized PEEP ventilation value was higher than the standard PEEP ventilation value.5-7
During OLV, reasonably individualized high PEEP ventilation can improve pulmonary oxygenation after alveolar ventilation, increase functional residual air volume, improve the ventilation/blood flow ratio, and prevent lung atrophy to counteract the effect of the patient position on respiratory mechanics.22, 23, 26-28
Pulmonary insufficiency resulting from low-tidal-volume settings can be effectively prevented by accelerating the respiratory rate and reducing the dead space volume, thereby reducing lung injury risk and improving lung function.6 Michela et al.13 titrated the optimal PEEP during OLV by using a PEEP decrement test, where the static respiratory system compliance (CRS) at each step was measured at the end of inspiration and expiration; the PEEP corresponding to the highest CRS was identified as the optimal PEEP. Such intraoperative adjustment of respiratory parameters according to the clinical situation is a reasonable ventilation strategy.29
On the basis of our findings, we concluded that surgery performed with a combined protocol of OLV with high PEEP + low tidal volume + high respiratory rate is an effective strategy for preventing pulmonary atelectasis. Our experimental data indicated a significantly lower degree of pulmonary atelectasis in the experimental group than in the control group.
Low tidal volume + continuous positive airway pressure ventilation provides positive pressure throughout the respiratory cycle during OLV, increases the functional residual air volume, maintains the airways and alveoli in a state of expansion during the expiratory phase, prevents alveolar atrophy, improves lung compliance and the ventilation/blood flow ratio, reduces the inflammatory response in both the lungs, and exerts a protective effect on lung function.30-32
Alveolar ventilation before OLV may reduce the degree of lung injury exacerbated through low tidal pulmonary resuscitation;7-10 The most commonly used method is manual ventilation before and after OLV, with continuous compression of the air sac enabling a slow increase of the peak airway pressure to 40 cmH2O for 10–15 s. However, different forms of pulmonary resuscitation can affect the degree of lung injury. Commonly used spirometric cardiopulmonary resuscitation or pressure maintenance cardiopulmonary resuscitation can cause a sharp increase in the right ventricular afterload, resulting in hemodynamic instability,33 which is harmful to alveolar capillary membranes.34 Periodic cardiopulmonary resuscitation using a slow stepwise increase in peak pressure and PEEP can reduce the degree of lung injury.35
Periodic cardiopulmonary resuscitation can be replaced by pressure-controlled ventilation before the patient is positioned laterally. A PEEP preinflation can first be administered to the ventilated lung to enable the lung to withstand pressure caused by the gravity factor of the position; further increasing the PEEP appropriately increases the alveolar pressure before the pleural cavity is opened on the operated side or before the positive pressure is administered to the pleural cavity on the operated side. The pressure maintains the expansion state of the alveoli for a short time, enabling the ventilated lung to withstand pressure caused by the loss of negative pressure and positive pressure in the pleural cavity. The following method maintains the constant driving pressure: the PEEP is increased by 5 cmH2O after every five breaths, and the driving pressure is adjusted to 20 cmH2O when the PEEP increases to 20 cmH2O, and perform ten consecutive breaths. Tests have verified that this method not only reduces the ineffective cavity volume but also improves oxygenation and ventilation efficiency, and this effect can last for the whole surgical procedure.36, 37
In terms of anesthetic drug selection, lowering the concentration of local anesthetics used reduces the occurrence of hypoxemia in OLV. After OLV in open-heart surgery, sevoflurane reduces ischemia–reperfusion injury in the lung more than isoproterenol, and desflurane exerts a greater effect on oxygen partial pressure than propofol.38-41
During surgery with OLV, an appropriate oxygen concentration can reduce the alveolar production of absorptive atelectasis and reperfusion injury caused by a high oxygen concentration.27 The inhalation oxygen concentration must be set at 0.5–0.8 as appropriate, and the inhalation oxygen concentration must be minimized intraoperatively to maintain the oxygen saturation at 92%–96%.22, 42
Airway secretion is a critical factor affecting intraoperative pulmonary atelectasis and must therefore be cleared as thoroughly as possible before OLV to prevent atelectasis on the ventilated side resulting from postural drainage. Preoperative and intraoperative humidification and appropriate nebulizing drugs can be administered to the ventilated lung to ensure that the alveoli and small airways are in a state of patency. Patients with poor pulmonary function or compliance should not undergo undergo nonintubated autonomic breathing surgery, especially for longer procedures, because they cannot effectively counteract intraoperative atelectasis caused by gravity, loss of negative pleural pressure, obstruction of secretion drainage, and redistribution of blood flow. These factors may increase the risk of intraoperative and postoperative complications, such as atelectasis on the ventilated side, and lung infection.
Our study indicates that the possibility of atelectasis in the ventilated side of the lung during lateral OLV in thoracic surgery is higher when protective ventilation strategies are used, and studies have demonstrated that intraoperative atelectasis can lead to lung injury and a series of postoperative complications. Different targeted ventilation strategies can prevent and improve intraoperative atelectasis during OLV, and combined with a series of effective measures can ensure the safety of intraoperative patients to a greater extent and effectively prevent postoperative complications.
Contributions: (I) Conception and design: GA, AA, MJ Ma, SQ Xu, B Han; (II) Provision of study materials or patients: H He, X Ma; (III) Collection and assembly of data: MJ Ma, SQ Xu, H He, X Ma; (IV) Data analysis and interpretation: MJ Ma, SQ Xu, B Han; (V) Manuscript writing: All authors; (VI) Final approval of manuscript: All authors.
Gianluca Ancona, Angelica Ancona, Shangqing Xu are contributed equally to this work as co-first authors.
Applicable Funding Source: 1. Gansu Provincial Key Research and Development Program - International Cooperation Field 24YFWA011
2. Science and Technology Program Project of Gansu Province: 23JRRA1597
Ethics number LDYYLL2022-476
References
1. Serpa Neto A, Hemmes SN, Barbas CS, et al. Incidence of mortality and morbidity related to postoperative lung injury in patients who have undergone abdominal or thoracic surgery: a systematic review and meta-analysis. Lancet Respir Med. 2014;2:1007-1015.
2. Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428-437.
3. Kozian A, Schilling T, Rocken C, Breitling C, Hachenberg T, Hedenstierna G. Increased alveolar damage after mechanical ventilation in a porcine model of thoracic surgery. J Cardiothorac Vasc Anesth. 2010;24:617-623.
4. Ladha K, Vidal Melo MF, McLean DJ, et al. Intraoperative protective mechanical ventilation and risk of postoperative respiratory complications: hospital based registry study. BMJ. 2015;351:h3646.
5. Della Rocca G, Coccia C. Acute lung injury in thoracic surgery. Curr Opin Anaesthesiol. 2013;26:40-46.
6. Kozian A, Schilling T, Schutze H, Senturk M, Hachenberg T, Hedenstierna G. Ventilatory protective strategies during thoracic surgery: effects of alveolar recruitment maneuver and low-tidal volume ventilation on lung density distribution. Anesthesiology. 2011;114:1025-1035.
7. Retamal J, Libuy J, Jimenez M, et al. Preliminary study of ventilation with 4 ml/kg tidal volume in acute respiratory distress syndrome: feasibility and effects on cyclic recruitment - derecruitment and hyperinflation. Crit Care. 2013;17:R16.
8. Szegedi LL, D'Hollander AA, Vermassen FE, Deryck F, Wouters PF. Gravity is an important determinant of oxygenation during one-lung ventilation. Acta Anaesthesiol Scand. 2010;54:744-750.
9. Spaeth J, Daume K, Goebel U, Wirth S, Schumann S. Increasing positive end-expiratory pressure (re-)improves intraoperative respiratory mechanics and lung ventilation after prone positioning. Br J Anaesth. 2016;116:838-846.
10. Choi YS, Bae MK, Kim SH, Park JE, Kim SY, Oh YJ. Effects of Alveolar Recruitment and Positive End-Expiratory Pressure on Oxygenation during One-Lung Ventilation in the Supine Position. Yonsei Med J. 2015;56:1421-1427.
11. Sivrikoz MC, Tuncozgur B, Cekmen M, et al. The role of tissue reperfusion in the reexpansion injury of the lungs. Eur J Cardiothorac Surg. 2002;22:721-727.
12. Leite CF, Calixto MC, Toro IF, Antunes E, Mussi RK. Characterization of pulmonary and systemic inflammatory responses produced by lung re-expansion after one-lung ventilation. J Cardiothorac Vasc Anesth. 2012;26:427-432.
13. Collins SR, Blank RS, Deatherage LS, Dull RO. Special article: the endothelial glycocalyx: emerging concepts in pulmonary edema and acute lung injury. Anesth Analg. 2013;117:664-674.
14. Lopez-Aguilar J, Piacentini E, Villagra A, et al. Contributions of vascular flow and pulmonary capillary pressure to ventilator-induced lung injury. Crit Care Med. 2006;34:1106-1112.
15. Meyhoff CS, Jorgensen LN, Wetterslev J, Christensen KB, Rasmussen LS, Group PT. Increased long-term mortality after a high perioperative inspiratory oxygen fraction during abdominal surgery: follow-up of a randomized clinical trial. Anesth Analg. 2012;115:849-854.
16. Wen ST, Chen W, Chen HL, et al. Amniotic fluid stem cells from EGFP transgenic mice attenuate hyperoxia-induced acute lung injury. PLoS One. 2013;8:e75383.
17. Pereira AL, Ferreira MR, Santos OJ, et al. Effects of oxygen in lungs of rats. Acta Cir Bras. 2014;29:771-775.
18. Chappell D, Heindl B, Jacob M, et al. Sevoflurane reduces leukocyte and platelet adhesion after ischemia-reperfusion by protecting the endothelial glycocalyx. Anesthesiology. 2011;115:483-491.
19. Ting Chen FW, Min Jiang. Research progress on the mechanism of lung injury associated with single lung ventilation in thoracic surgery. Jiangxi Medical Journal. 2017;52.
20. Jeon K, Yoon JW, Suh GY, et al. Risk factors for post-pneumonectomy acute lung injury/acute respiratory distress syndrome in primary lung cancer patients. Anaesth Intensive Care. 2009;37:14-19.
21. Shen Y, Zhong M, Wu W, et al. The impact of tidal volume on pulmonary complications following minimally invasive esophagectomy: a randomized and controlled study. J Thorac Cardiovasc Surg. 2013;146:1267-1273; discussion 1273-1264.
22. Brassard CL, Lohser J, Donati F, Bussieres JS. Step-by-step clinical management of one-lung ventilation: continuing professional development. Can J Anaesth. 2014;61:1103-1121.
23. Spadaro S, Grasso S, Karbing DS, et al. Physiologic Evaluation of Ventilation Perfusion Mismatch and Respiratory Mechanics at Different Positive End-expiratory Pressure in Patients Undergoing Protective One-lung Ventilation. Anesthesiology. 2018;128:531-538.
24. El Tahan MR, Pasin L, Marczin N, Landoni G. Impact of Low Tidal Volumes During One-Lung Ventilation. A Meta-Analysis of Randomized Controlled Trials. J Cardiothorac Vasc Anesth. 2017;31:1767-1773.
25. Blank RS, Colquhoun DA, Durieux ME, et al. Management of One-lung Ventilation: Impact of Tidal Volume on Complications after Thoracic Surgery. Anesthesiology. 2016;124:1286-1295.
26. Ferrando C, Mugarra A, Gutierrez A, et al. Setting individualized positive end-expiratory pressure level with a positive end-expiratory pressure decrement trial after a recruitment maneuver improves oxygenation and lung mechanics during one-lung ventilation. Anesth Analg. 2014;118:657-665.
27. Liu J, Liao X, Li Y, et al. Effect of low tidal volume with PEEP on respiratory function in infants undergoing one-lung ventilation. Anaesthesist. 2017;66:667-671.
28. Hoftman N, Canales C, Leduc M, Mahajan A. Positive end expiratory pressure during one-lung ventilation: selecting ideal patients and ventilator settings with the aim of improving arterial oxygenation. Ann Card Anaesth. 2011;14:183-187.
29. Slinger PD. Do Low Tidal Volumes Decrease Lung Injury During One-Lung Ventilation? J Cardiothorac Vasc Anesth. 2017;31:1774-1775.
30. Verhage RJ, Croese AC, van Hillegersberg R. Reduced local immune response with continuous positive airway pressure during one-lung ventilation for oesophagectomy. Br J Anaesth. 2015;114:1009-1010.
31. Grichnik KP, Shaw A. Update on one-lung ventilation: the use of continuous positive airway pressure ventilation and positive end-expiratory pressure ventilation--clinical application. Curr Opin Anaesthesiol. 2009;22:23-30.
32. Kim YD, Ko S, Kim D, Lim H, Lee JH, Kim MH. The effects of incremental continuous positive airway pressure on arterial oxygenation and pulmonary shunt during one-lung ventilation. Korean J Anesthesiol. 2012;62:256-259.
33. Marini JJ. Recruitment by sustained inflation: time for a change. Intensive Care Med. 2011;37:1572-1574.
34. Silva PL, Moraes L, Santos RS, et al. Recruitment maneuvers modulate epithelial and endothelial cell response according to acute lung injury etiology. Crit Care Med. 2013;41:e256-265.
35. Yang W, Wei K, An Y, et al. [Effect of unilateral lung recruitment maneuver on hemodynamics and dead space ratio in pigs with unilateral acute respiratory distress syndrome]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2014;26:554-557.
36. Verhage RJ, Boone J, Rijkers GT, et al. Reduced local immune response with continuous positive airway pressure during one-lung ventilation for oesophagectomy. Br J Anaesth. 2014;112:920-928.
37. Tojo K, Goto T, Kurahashi K. Protective effects of continuous positive airway pressure on a nonventilated lung during one-lung ventilation: A prospective laboratory study in rats. Eur J Anaesthesiol. 2016;33:776-783.
38. Ng A, Swanevelder J. Hypoxaemia associated with one-lung anaesthesia: new discoveries in ventilation and perfusion. Br J Anaesth. 2011;106:761-763.
39. Erturk E, Topaloglu S, Dohman D, et al. The comparison of the effects of sevoflurane inhalation anesthesia and intravenous propofol anesthesia on oxidative stress in one lung ventilation. Biomed Res Int. 2014;2014:360936.
40. Cho YJ, Kim TK, Hong DM, Seo JH, Bahk JH, Jeon Y. Effect of desflurane-remifentanil vs. Propofol-remifentanil anesthesia on arterial oxygenation during one-lung ventilation for thoracoscopic surgery: a prospective randomized trial. BMC Anesthesiol. 2017;17:9.
41. Beck-Schimmer B, Bonvini JM, Braun J, et al. Which Anesthesia Regimen Is Best to Reduce Morbidity and Mortality in Lung Surgery?: A Multicenter Randomized Controlled Trial. Anesthesiology. 2016;125:313-321.
42. Okahara S, Shimizu K, Suzuki S, Ishii K, Morimatsu H. Associations between intraoperative ventilator settings during one-lung ventilation and postoperative pulmonary complications: a prospective observational study. BMC Anesthesiol. 2018;18:13
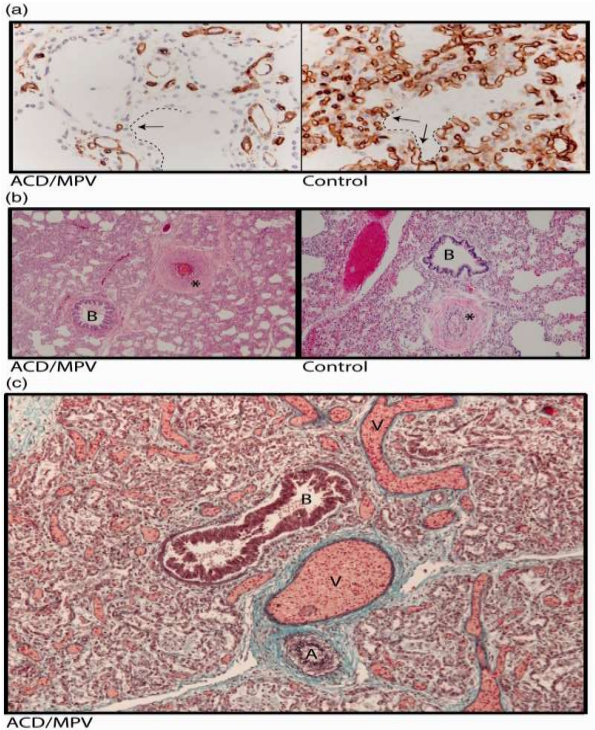
Figure 1
