Hepatic Hydatid Cyst : A Combined Open And Laparoscopic Surgical Approach
Hepatic Hydatid Cyst : A Combined Open And Laparoscopic Surgical Approach
Aman Siloiya MBBS 1, Sanjeev Gupta MBBS, MS1, Ajay Jawahar MBBS MS FACS 1*
1. Department Of General Surgery, Dr. KNS Memorial Institute of Medical Sciences , Barabanki (Formerly Known As Mayo Institute Of Medical Sciences), Barabanki, Uttar Pradesh, India.
*Correspondence to: Ajay Jawahar MBBS MS FACS, Department Of General Surgery, Dr. KNS Memorial Institute of Medical Sciences , Barabanki (Formerly Known As Mayo Institute Of Medical Sciences), Barabanki, Uttar Pradesh, India.
Copyright
© 2025 Dr. Ajay Jawahar, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 07 July 2025
Published: 23 July 2025
Abstract:
Cystic Echinococcosis (CE) is a widely endemic helminthic disease caused by infection with metacestodes (larval stage) of the Echinococcus granulosus tapeworm. E. granulosus are common parasites in certain parts of the world, and are present on every continent with the exception of Antarctica. Surgery continues to be the hallmark of the definitive treatment but opinions still differ as to the best surgical technique. We report a novel approach to combine laparoscopic with conventional surgery in an attempt to minimize the chances of recurrence in a young female with CE of liver.
Hepatic Hydatid Cyst : A Combined Open And Laparoscopic Surgical Approach
Introduction
Human cystic echinococcosis, or hydatid cyst disease, is a zoonosis caused by the larval cestode Echincoccus granulosus. Dogs are the definitive hosts for Echinococcus granulosus and sheep the major intermediate host (yaks, goats, and camels are other relevant intermediate hosts); man is only incidentally infected. The liver is the most frequent site for the cystic lesions seen in hydatid disease, followed by the lung, brain, and other viscera. The goals of surgery in hydatid disease are to inactivate the cestode parasites, evacuate the cyst cavity, remove the germinal layer, and obliterate the residual cavity.
A large number of people are affected by CE every year throughout the world. The increased emigration of populations from endemic areas where prevalence rates are as high as 5–10% and the relatively quiescent clinical course of CE pose challenges for accurate and timely diagnoses. Upon infection with CE, cyst formation mainly occurs in the liver (70%). Diagnosis involves serum serologic testing for antibodies against hydatid antigens, but preferably with imaging by ultrasound or CT/ MRI.(3,4) Liver Hydatidosis cannot properly be considered a “benign disease” as it is progressive, often recurrent (10% to 20% of cases)(5) , may cause life threatening complications, and carries a mortality rate that reaches 10% in recurrences. The disease is characterized by the progressive growth of the hydatid cyst, which in its mature form is a fluid- filled cavity, delimitated by an external dense host fibrous reaction (pericyst) and two internal parasite-derived layers (endocyst).
Surgical interventions consist of conservative, radical, and laparoscopic approaches. Meticulous packing of the operative field is necessary irrespective of the surgical technique employed. Potential major complications associated with the surgical treatment of hepatic hydatid cysts include postoperative hemorrhage, bile exudation from the residual cyst cavity, incisional fistula formation, cholangitis, wound infection, sepsis, incisional fistulae, pulmonary complications such as pneumonia and pulmonary embolization, complications of anesthesia, and death. We hereby present our experience of excision of hepatic hydatid cyst in which both open surgical approach as well as laparoscopic instrumentation was used in order to assure removal of all the daughter cysts from within the primary endocyst and the surrounding perihepatic area.
History and Physical Examination
A 21 year female came to OPD with complaints of pain in the right upper abdomen and nausea by herself since past 3-4 months. Pain was of insidious onset, gradually progressive, dull aching, moderate in intensity, gets relieved on taking medications, associated with fever and chills. She had normal menarche with no family history of cystic diseases. She did not report ingesting any oral contraceptive pills.
Physical examination revealed tenderness in the right hypochondrium
Radiology
Ultrasonogram of the whole abdomen revealed a well defined anechoic cystic lesion (measuring 8.55 x 8.2 x 7.9 ) containing ( 280-300 cc) is seen in the segment VI , VII , VIII with thick septations, other smaller cysts were also detected surrounding the primary cyst.(Figure 1).
Figure 1 – Ultrasonogram picture of the abdomen showing primary and daughter cysts
Surgical Procedure
The procedure was planned under general anesthesia. An approximately 8 cm right subcostal skin incision was given. Abdomen was opened in layers after liver and Gall bladder identification, the cysts were palpated gently. The liver was mobilized and packed all around with gauge soaked in a mixture of chlorhexidine and saline. The primary cyst was visualized and drained with a wide bore needle. The exocyst membrane was incised and endocyst was accessed. Approximately 12-13 daughter cysts were detected within the cavity and were carefully removed without rupturing (Figure 2). Considering the multiplicity, very small size and deep posterior location of the daughter cysts, a laparoscope camera was introduced into the cavity to thoroughly explore the cavity for more cysts. This maneuver revealed 10 more, smaller cysts that were not previously seen with the naked eye inspection (Figure 3). These also were carefully removed and the cavity was inspected for any biliary leakage. The endocyst was removed intact. A thorough lavage of the cavity was done and a pedicled omental patch isolated and filled in cavity of the cyst. Two drains were placed in sub hepatic pouch and sub diaphragmatic space. Abdomen was closed in layers.
Figure 2- Intraoperative Image showing intact pericyst and multiple daughter cysts
Figure 3- Laparoscopic camera image within the endocyst cavity showing multiple daughter cysts previously undetected by the naked eye
Histopathological Examination
HPE revealed large ruptured cyst along with multiple small fluid filled daughter cyst altogether measuring 18x10x2.5 cm. Largest ruptured cyst measures 14x9.2.5 cm. Cyst wall thickness was 0.4 cm. Smallest cyst measuring 1x1 cm. On cut section of intact cyst, clear fluid oozed out. Microscopic H&E staining revealed thick eosinophilic laminated layer along with degenerated inner germinal layer. Sections from daughter cyst revealed numerous mature and degenerated proctoscolices along with hooklets suggestive of Hydatid disease of Liver.
Discussion
Hydatid disease of the liver due to Echinococcus granulosis remains as an important and challenging medical problem (4).It has a worldwide distribution and is endemic in many countries but because of increased immigration and traveling, the disease has now become more frequent outside endemic areas(1). Although surgery is unanimously considered the treatment of choice for hydatid disease of the liver, controversies still exist about the preferred operative technique. (6)
Liver hydatidosis may cause life threatening complications, and carries a mortality rate that reaches 10% in recurrences. The disease is characterized by the progressive growth of the hydatid cyst, which in its mature form is a fluid-filled cavity, delimitated by an external dense host fibrous reaction (pericyst) and two internal parasite-derived layers (endocyst). The hydatid cyst slowly enlarges in the liver and usually remains asymptomatic for many years. Symptoms arise either when the cyst has grown enough to cause pressure on adjacent organs or when a complication occurs. Infection and intrabiliary rupture are the most common complications. (7).
The use of medications, ie, benzimidazole compounds, to treat established echinococcal liver cysts remains disappointing." (8)(9). Although the efficacy of high-dose mebendazole or albendazole has been reported in some cases, little objective evidence exists to support these claims; low concentrations of active drug were found at surgery in cystic fluids of patients receiving long-term preoperative medical treatment, and persistence ofliving parasites within the cysts was document¬ ed in more than half of the patients (10). A recent multicenter study conducted by the World Health Organization has suggested that medical treatment be restricted to inoperable cases or to the prevention of postoperative recurrences (11).
Surgery thus remains the primary treatment for hydatid liver cysts. There is, however, considerable disagreement about the preferred surgical technique. The major issue of debate is whether complete removal of the pericyst is necessary to cure the disease properly and thus whether conservative or radical procedures should be favored (12).
Complete removal of the pericyst should allow the achievement of two main goals: (1) a lower rate of postoperative complications, by reducing the incidence of biliary leakage (13); and (2) a lower rate of recurrence, by allowing detection and correct treatment of exogenous daughter cysts. About the first point, biliary leakage is known to be the most frequent postoperative complication following surgery for hydatid liver disease. It has been reported to occur in as many as 50% of patients as a consequence of small, undetected communications between the cyst and the bile ducts. It may lead to external biliary fistula or abscess formation that remarkably prolongs the hospital stay and occasionally requires reoperation. When conservative procedures are used, persistence of the pericystic layer, particularly if thick and calcified, may disguise biliary communications in the residual cavity. On the contrary, with complete dissection of the pericyst, biliary pedicles communicating with the cyst are more easily identified and safely ligated in the healthy parenchyma.
With the increase in the number of laparoscopic interventions as a result of the application of current technology to liver surgery, laparoscopic treatment of cysts located close to the surface has become possible, especially in the inferior-anterior segments that are easy to access. In our study, surgery was started laparoscopically in 79 patients. Conversion to open surgery was performed in 18 cases. Difficulty in reaching the cyst, anatomical localization of the cyst, bleeding, and long learning curve can be counted as the causes of conversion. In our study, the laparoscopic procedure was successfully applied to 61 patients. (14)
The most common techniques for liver hydatid disease treatment are marsupialization, partial cystopericystectomy with resection of the pericyst and subtotal pericystectomy by peeling the pericystium. (15)
Both laparoscopic and open approaches are safe and effective. The results are similar and comparable, and many of the open-surgery cases could be done laparoscopically if patients are properly selected. Recurrent, multiorgan hydatid cysts, multiple liver cysts, huge cysts with suspected major biliary communication, deep intraparenchymal located cysts, and those present in the blind area for laparoscopy in segments 1 and 7, are better to be managed by open surgery (16).
Local recurrence represents a major concern in hydatid liver disease. Better understanding of the mechanisms of daughter cyst formation has shed new light on this problem.8,19 As the hydatid cyst enlarges, small aggregations of cells bulge from the inner layer of the endocyst (germinal epithelium) within the main cavity to form endogenous daughter cysts (Fig 1, top, white arrow). In some cases, the germinal epithelium also protrudes toward the external side of the cyst, to form exogenous daughter cysts. This phenomenon seems to occur more frequently than previously suspected. Tagliacozzo et al. in his series of 97 total cystopericystectomies, found 22 cases (23%) (13). However, the literature remains very sparse in surgical approaches employing a combined open and laparoscopic approach for the removal of hepatic hydatid cyst with multiple daughter cysts embedded within the primary cyst and neighbouring liver parenchyma. This is what makes our case report different from the existing literature and can be a guideline for surgeons approaching such difficult surgical dilemma.
Conclusion
Hepatic hydatid cysts continue to pose a surgical challenge because of the problem of multiple daughter cysts and high recurrence rate. The individual philosophy of the surgeons continues to be the deciding factor regarding the surgical approach to be taken. However, no published literature provides a definitive guideline regarding the best approach. This reason motivated us to try this novel surgical approach that combined open as well as laparoscopic techniques to minimize the chances of recurrence due to remaining daughter cysts. We will continue to follow this patient carefully on a longer term basis to early detect any evidence of recurrence.
References
1. Eckert J, Gemmel MA, Matyas Z, Saulsby EJ. Guidelines for Surveillance Prevention and Control of Echinococcosis/Hydatidosis. Geneva, Switzerland: World Health Organization; 1984;VPH/81.28:1-5.
2. (Treatment options for hepatic cystic Echinococcosis Raymond A. Smego Jr.*, Peter Sebanego doi:10.1016/j.ijid.2004.08.001)
3. (Hepatic Echinococcal Cysts: A Review Tina Pakala1, Marco Molina2 and George Y. Wu*1 DOI: 10.14218/JCTH.2015.00036)
4. Surgical Treatment of Hydatid Disease of the Liver Paolo Magistrelli, MD; Riccardo Masetti, MD; Roberto Coppola Arch Surg. 1991;126:518-523))
5. Little JM, Hollands MJ, Ekberg H. Recurrence of hydatid disease. World J Surg. 1988;12:700-704.) ( 12. Mottaghian H, Saidi F. Post-operative recurrence of hydatid disease. BrJSurg. 1978;65:237-242.
6. Belli L, Aseni P, Rondinara GF, Bertini M. Improved results with pericystectomy in normothermic ischemia for hepatic hydatidosis. Surg Gynecol Obstet. 1986;163:127-132)
7. Sayek I, Yalin R, Sanac Y. Surgical treatment of hydatid disease of the liver. Arch Surg. 1980;115:847-850.)
8. Davis A, Pawlowski ZS, Dixon H. Multicentre clinical trials of benzimidazole carbamates in human echinococcosis. Bull WORLD Health Organ. 1986;64:383-388.) "
9. Pitt HA, Korzelius J, Tompkins RK. Management of hepatic echinococcosis in Southern California. AmJSurg. 1986;152:110-115.)
10. Schantz PM. Effective medical treatment for hydatid disease? JAMA. 1985;253:2095-2097.)
11. Davis A, Pawlowski ZS, Dixon H. Multicentre clinical trials of benzimidazole carbamates in human echinococcosis. Bull WORLD Health Organ. 1986;64:383-388.
12. Morel P, Robert J, Rohner A. Surgical treatment of hydatid disease of the liver: a survey of69 patients. Surgery. 1988;104:859-862.
13. Tagliacozzo S. Typical and atypical resections in the surgical treatment of hydatid disease of the liver. Surg Italy. 1977;7:133-138.
14. (Öter and Yalç?n. Emergency in Liver Hydatid Cysts Turk J Gastroenterol 2023; 34(10): 1071-1077)
15. (Modified capitonage in partial cystectomy performed for liver hydatid disease: Report of 2 cases Dimitrios K Filippou*1, Chariton Kolimpiris2, Nikolaos Anemodouras3 and Spiros Rizos1 : BMC Surgery 2004, 4:8 doi:10.1186/1471-2482-4-8).
16. Laparoscopic versus open surgical management of liver hydatid cyst: a retrospective study Ahmed S.M. Omar, Tarek A. Osman, Mohab G. El Barbary The Egyptian Journal of Surgery 2022, 41:65–75.
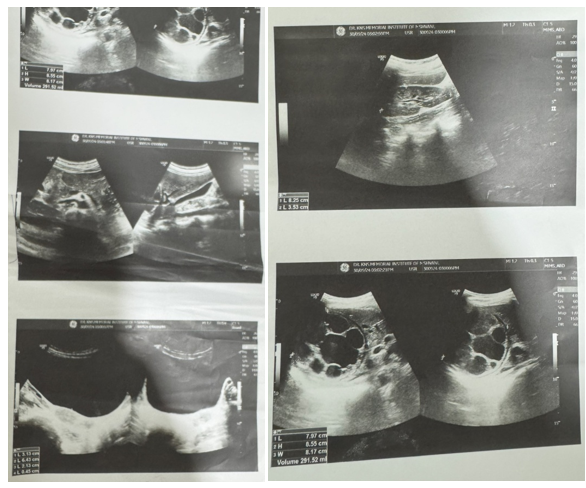
Figure 1

Figure 2

Figure 3
